Chronic liver disease is currently the fifth largest killer in the world. After serious damage occurs, the liver loses its ability to repair itself thus giving rise to a life-threatening condition. The only treatment that was thought to be available was a liver transplant. Would regenerative medicine be able to help?
The liver is a multifaceted organ that plays a role in digestion, blood sugar control, blood clotting factors for healing, making amino acids, increasing red blood cell growth, fat and cholesterol transport and the removal of waste, especially toxic exposures and the metabolization of medications into their active ingredients.
The majority of the liver (80 %) is made up of highly specialized cells called hepatocytes. These cells have an average lifespan of 150 days as the liver is constantly renewing itself under healthy conditions. It is the only organ in the body that can easily replace damaged cells, but if are large amount of healthy cells are lost, the liver may not be able to meet the needs of the body, leading to liver failure.
Causes of Liver Disease:
- Hepatitis: viral, toxic, autoimmune or hereditary conditions.
- Alcoholic liver disease including fatty liver disease, alcoholic hepatitis and cirrhosis.
- Fatty liver disease may lead to inflammatory disease and then to cirrhosis.
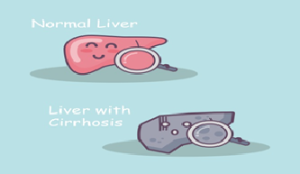
- Cirrhosis is the formation of fibrous tissue in the place of dead liver cells and causes chronic liver failure.
- Primary liver cancer.
- Primary biliary cirrhosis is a serious autoimmune disease of the bile capillaries.
- Primary sclerosing cholangitis.
- Budd-Chiari syndrome caused by occlusion of the hepatic vein, which in some cases may lead to cirrhosis.
- Hereditary diseases (hemochromatosis, involving accumulation of iron in the body, and Wilson’s disease, which causes the body to retain copper, Alfa 1-antitripsin deficiency and glycogen storage disease type II).
- Transthyretin-related amyloidosis.
- Gilbert’s syndrome.
Cirrhosis is a term that describes permanent scarring of the liver. Normal liver cells are replaced by scar tissue that cannot the required perform the required bodily functions. Acute liver failure could be life threatening and at one time it was believed to be irreversible but stem cell regeneration has proven most effective.
Liver disease can progress to cirrhosis and liver failure. Complications include increased risk of bleeding, infection, malnutrition, weight loss, decreased cognitive function over time and an increased risk of cancer.
Reinforcing therapies have the potential to save us from conditions of day-to-day survival to ones in which we can hope for a better quality of life. Medical research area of stem cells and regenerative medicine is moving fast, providing hope of life to millions of patients and their families, worldwide.
Treatment of liver options
Although the liver can recover and restore its function, there are no warning signs that it is failing until too late. Once the chronic liver disease or the final stage or liver failure, is reached, there are fewer options. There is no “liver dialysis” that can rehabilitate liver function yet.
Until now, transplantation was the only effective treatment for liver failure, but it has many drawbacks, including the risk of rejection, risks associated with surgery, and donor shortage. Many people die from end-stage liver disease waiting for a donor organ.
Many patients with acute liver failure have received hepatocyte transplants from cadaveric donors, with some improvement in liver function, but the effects were short lived with no overall survival benefit. The major challenges with this approach was shortage of cadaveric donors and immune suppression of patients which is the same as for whole organ transplants.
How can St em Cell Therapy help in the treatment of liver diseases?
em Cell Therapy help in the treatment of liver diseases?
Today, autologous adipose tissue stem cells are the major type of stem cells that have been used clinically for treating liver disease. The big advantage with using these cells is that because they come from the patient, there is no risk of rejection when they are transplanted back. The stem cells are transdifferentiating into hepatocytes as well as producing soluble factors that promote regeneration and repair with the possibility that the stem cells may be fusing with resident hepatocytes to direct their regeneration.

Recent Comments